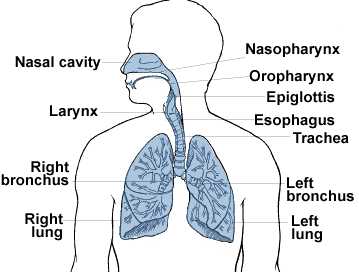
TYPES OF LUNG CANCER
There are important differences
between lung cancer that started in the lungs and lung cancer
that has spread to the lung. This section is about primary
lung cancer - cancer that started in the lungs. There are
several different types of primary lung cancer. These are
divided into two main types:
- Small cell lung cancer
- Non-small cell lung cancer
There is another rare type of
cancer called
mesothelioma that affects the
covering of the lung (the pleura). It is often caused by
exposure to asbestos. It is very different to lung cancer.
Small cell lung cancer
Small cell lung cancer is so called because the cancer cells are
small cells that are mostly filled with the nucleus (the control
centre of cells). Small cell lung cancer often spreads
quite early on.
Non-small cell lung cancer
There are four types of non-small cell lung cancer. These are
grouped together because they behave in a similar way and
respond to treatment differently to small cell lung cancer. The
four types are:
- Squamous cell carcinoma
- Adenocarcinoma
- Large cell carcinoma
- Epidermoid carcinoma
Occasionally it is not possible
to work out which type of non small cell lung cancer you have.
If the cells in the biopsy are very undeveloped, it just may not
be possible to tell.
Squamous cell cancer is the commonest type of lung cancer. It
develops from the cells that line the airways. The
incidence of squamous cell cancer is going down in the UK.
Adenocarcinoma also develops from the cells that line the airways.
But it develops from a particular type of cell that produces
mucus (phlegm). The incidence of adenocarcinoma is
increasing and it may soon become more common in the UK than
squamous cell lung cancer.
Large cell lung cancer is called this because the cells look large
and rounded when they are looked at under a microscope.
Epidermoid carcinomas are most
common among men and the elderly. It starts in one of the larger
breathing tubes and usually does not grow or spread as quickly
as other types of lung cancer.
How does epidermoid carcinoma develop?
Non-small cell lung cancer is usually associated with a history of
smoking, passive smoking or radon exposure. More than 87 percent
of lung cancers are caused directly by smoking, while some of
the remainder is caused by environmental exposure to tobacco
smoke. Other risk factors for lung cancer include a family or
personal history of lung cancer and exposure to cancer-causing
agents in the workplace or the environment. Asbestos workers are
about seven times more likely to die of lung cancer compared to
the general population. Exposure to asbestos fibres is an
important risk factor for lung cancer. Asbestos workers who
smoke have a 50 to 90 times greater chance of getting lung
cancer than that of the population in general. Radon, a
radioactive gas that occurs when uranium breaks down naturally,
cannot be seen, tasted, or smelled. It can become more
concentrated indoors and may pose a cancer risk. Studies from
populated areas in parts of the United States built over soil
with natural uranium deposits have found that the risk of lung
cancer may be doubled or even tripled after one has lived in a
radon-contaminated residence for an extended period of time.
However, when compared to the lung cancer risk associated with
tobacco, the radon risk cited in the example above is very
small.
What are the symptoms of epidermoid carcinoma?
Although some cancers do not have any symptoms at first, this type
of cancer is diagnosed because of complaints such as a
persistent cough, coughing up of blood, shortness of breath or
wheezing, unexplained weight loss or loss of appetite, fatigue,
difficulty swallowing, pain in the chest, shoulder or arm,
recurrent pneumonia in the same place, bone pain, hoarseness,
headaches, confusion or seizures and swelling of the face, neck
or upper extremities.
Cancer that has spread to the lungs
Secondary cancer is cancer that has spread from somewhere else in
the body. There are quite a few different cancers that can
spread to the lungs, including breast cancer and bowel cancer.
It is important to know what you are dealing with so that you can
find the right information. The choice of cancer treatment
depends on where the cancer started. When cancer spreads
to the lung from the breast, the cells are breast cancer cells,
not lung cancer cells. So they respond to breast cancer
treatments. And cancer that has spread from the bowel should
respond to bowel cancer treatments.
Mesothelioma see
website:
www.mesothelioma.uk.com
Mesothelioma is a cancer
occurring in the lining of the lungs, chest and abdomen. The only known cause of
mesothelioma is exposure to asbestos products. The risk of developing
mesothelioma varies, depending on duration and intensity of exposure.
Malignant mesothelioma
affecting the lungs and chest cavity is referred to as "pleural mesothelioma".
When the disease affects the abdominal cavity, it is referred to as "peritoneal
mesothelioma". A more detailed discussion of both types of malignant
mesothelioma appears later in this book.
Mesothelioma generally begins
in the lungs and spreads to the abdominal lining. The prognosis worsens when the
abdominal lining becomes affected. In most cases, death is the result of the
invasive nature of the tumour on heart and/or lungs.
Asbestos exposure is generally
a common factor uniting mesothelioma victims.
Patients are generally male
(over 80%).
Typical symptoms include chest
pain, shortness of breath, coughing, weight loss, and sexual dysfunction. In
later stages of the disease process, patients may experience deformation of the
chest wall and abdominal masses that may or may not obstruct the bowel.
There is as yet no known cure
for malignant mesothelioma. The prognosis depends on various factors, including
the size and stage of the tumour, the extent of the tumour, the cell type, and
whether or not the tumour responds to treatment. The individual mesothelioma
victims age and state of underlying health, as well as their state of mind and
motivation to survive the disease likewise may play a role in a favourable
prognosis.
Although there is no standard
treatment protocol for mesothelioma, numerous treatment options are available
for those diagnosed with the disease. Early diagnosis typically results in a
greater range of available treatment options. Treatments include:
- traditional chemotherapy
- radiation therapy
- surgery
- experimental therapies and drugs
- complementary medicine and therapies
- lifestyle modifications
Traditional Chemotherapy
In traditional chemotherapy,
special anti-cancer (cytotoxic) medicines and chemicals are administered, with
the goal of killing the malignant cells. Chemotherapy is frequently one facet of
a regimen including radical surgery, radiation therapy and/or immunotherapy.
Chemotherapy may also be used in situations where the cancer has spread to the
extent that surgery is no longer a viable option.
Many drugs have been tried;
however all have met with only limited success against malignant mesothelioma.
The response rate to single agent chemotherapy is typically less than 20%; use
of drug combinations yields little difference in result. There is therefore no
standard of systemic chemotherapy for the treatment of mesothelioma.
The chemotherapeutic agents
can be administered either systemically (in the blood stream) or intra-pleurally
(in the pleural cavity itself.) These cytotoxic drugs are very potent. Because
they cannot differentiate healthy cells from cancerous ones, they often have
many severe side effects.
Radiation Therapy
(Radiotherapy)
Radiation therapy involves the
localized use of high-dose radiation (like x-rays) on malignant tumours.
Typically, radiation therapy not used on its own, but rather, in conjunction
with other therapies such as surgical resection and chemotherapy. In many
instances, the potential benefit that may be gained from radiation is outweighed
by side effects, including radiation pneumonitis, myelitis, hepatitis and
myocarditis, which may significantly diminish the patients quality of life.
Radiation can also be used for palliative (pain-relieving) purposes--to reduce
the tumours size, thereby helping to relieve symptoms like pain and shortness of
breath.
Factors that can limit the
application of radiation as a treatment method include the volume of the tumour
and how near it is to vital organs. Compared to other types of
lung cancer in terms of how it responds to radiation, mesothelioma is not as
sensitive to radiation as small cell carcinoma of the lung, but may be more
responsive to radiation treatment than non-small cell lung cancer.
Exploratory surgery
Exploratory surgery of the
chest (thoracoscopy or thoracotomy), can be a valuable tool in early diagnosis
of mesothelioma. If the disease is detected early, the patient has more
treatment options to consider, including the potential for aggressive surgery.
During an exploratory
procedure, doctors may also drain built-up fluid from pleural effusions.
Drainage may help to alleviate shortness of breath, but is regarded as
essentially a palliative measure. Drainage may not be effective, however, where
the patient has a bulky tumour in the pleural space or where a thick visceral
pleural peel of tumour confines the lung.
Surgical treatments
Extra-pleural
pneumonectomy (EPP)
EPP is regarded as radical
surgery. It is a major surgical procedure, involving removal of the pleura,
diaphragm, pericardium, portions of the phrenic nerve, and the whole lung
affected by the tumour.
To increase the rate of
survival, EPP must be followed by adjuvant therapy (chemotherapy and/or
radiation), and it carries a significant risk (greater than 15%) of death during
or shortly after surgery. Its application is therefore typically confined to a
minority of patients who are in Stage I of the disease and who are otherwise
medically fit to undergo major surgery.
Pleurectomy/decortication
Pleurectomy/decortication
involves the removal of the pleura÷essentially, surgically stripping the pleura
and pericardium from the apex of the lung to the diaphragm--but without removing
the entire lung. This procedure offers the best option for locally controlling
pleural fluid. The Cause of death is much less than with EPP (under 3%).
Pleurectomy is regarded as more effective than talc pleurodesis in reducing the
recurrence of pleural effusion associated with mesothelioma.
Pleurecotomy is best used in
patients who are managing their disease generally and have good expansion in
their lungs, but who have experienced rapid and symptomatic fluid build-up.
Pleurectomy may also be a more suitable treatment method for mesothelioma
sufferers in later stages of the disease than the more radical and risky EPP, as
well as for older mesothelioma sufferers.
Surgery can remove the bulk of
the tumour and provide symptomatic relief÷but it is not a viable option if the
tumour is near vital organs. Both EPP and pleurectomy/decortication are complex
surgeries, not performed frequently by most surgeons, and require referral to
centres dedicated to such treatment. Many of these centres also specialize in
other forms of mesothelioma treatment, alone or in combination (multi-modal
therapy.)
Which type of surgery is
recommended depends on many factors, including the stage of the tumour. Notably,
in at least one study, researchers found that the size of the tumour prior to
surgery was a good predictor of surgical outcome and overall survival.
Mesothelioma sufferers should
evaluate all options carefully, since no one procedure has been comprehensively
shown to have distinct advantages over another. Further, surgery has not been
shown to offer significant advantages over non-surgical options.
Experimental drugs
Onconase
Onconase, made by
pharmaceutical company Alfacell, has shown a survival benefit to sufferers of
malignant mesothelioma in a study, the results of which were released in March
1999. The study showed a 34.3% one-year survival rate and 21.1% two-year
survival rate to patients with inoperable malignant mesothelioma. Another study
of Onconase is expected to compare its results with those of doxorubicin, a
standard chemotherapy drug.
Onconase is an enzyme derived
from purified frog eggs. The enzyme degrades RNA, which is used by cells to
produce protein and energy.
The successful study discussed
above monitored 105 mesothelioma patients, all of whom received weekly infusions
of Onconase until their cancers failed to respond to the drug. Of these
patients, 39% demonstrated either reduction of tumour size or stabilization of
the disease, as measured by CT scan. Of this 39%, the mean survival time was
over 17 months; 61% of that group survived for a year, and 31.7% survived two
years. Even among those with the negative prognostic indicator of abdominal
involvement, there was a mean survival rate of 12 months, a 1-year survival rate
of 48% and a 2-year survival rate of 35.6%.
One unexplained, but
potentially positive finding of the study is that patients with abdominal
involvement typically a sign that the disease is worsening actually had a better
outcome than those without abdominal involvement in the disease process.
Patients in this study
generally tolerated the drug well, with only five dropping out of the study due
to side effects. Typically experienced side effects were kidney problems,
swelling of the extremities and rashes.
A 1996 study of Onconase
effects on mesothelioma yielded similar results. In that study, 20 patients with
malignant mesothelioma were treated with the drug. Three patients demonstrated
partial responses that is, they showed a greater than 50% reduction in the size
of their tumours. Ten patients showed stabilization of the progress of their
mesothelioma which had been progressing prior to use of Onconase.
Lovastatin
Lovastatin, a drug that is
typically tolerated well by users, and that has been widely used in the
treatment of high cholesterol, has shown positive results in inhibiting
mesothelial cell growth. This drug has not yet been subjected to clinical
trials, however.
Endostatin and
angiostatin
Another promising treatment
regimen involves endostatin and angiostatin, substances that inhibit the growth
of the blood vessels that feed cancerous tumours. Cancers like mesothelioma (as
well as breast cancer, melanoma, and kidney cancer) typically need many blood
vessels to grow. Use of endostatin and angiostatin inhibits the growth of the
blood vessels that feed the tumour, thereby slowing or inhibiting the disease
process.
Immunotherapy
Immunotherapy is based on the
theory that the body's own immune defences can be mobilized to fight against
cancerous cells. Several experimental treatments seek to enhance the immune
system's ability to combat malignant mesothelioma. These include gene therapy
and the use of cytokine proteins such as interferons and interleukin-2. These
treatments are being tested both alone and in combination with other treatments
such as chemotherapy.
Gene therapy
Gene therapy changes the
genetic machinery of the cancer cells. The cells are initially infected with
"suicide genes," delivered to them by adenoviruses (viruses that cause colds and
herpes). The viruses used for gene therapy are disabled and packed with an
enzyme, which turns into a poison and cripples the cell's genetic machinery
thereby stopping the rapid division of the cancer cells and thus inhibiting
rapid growth of the mesothelial tumour. This therapy, which has been
successfully used for sufferers of both mesothelioma and brain cancer, may
require surgery as well as careful monitoring.
Notably, gene therapy may be
better suited to mesothelioma patients than other cancer sufferers. For example,
mesothelioma patients are able to tolerate higher doses of the adenoviruses than
brain cancer sufferers, and this therapy has not adversely affected the small
number of mesothelioma sufferers upon whom it has been implemented. There is no
evidence, however, that this therapy reduced the size of mesothelial tumours.
Rather, its effect appears to be retardation of tumour growth.
Gene therapy allows for
treatment that specifically targets only the tumour. In fact, researchers are
studying a vaccine that could be injected directly into the tumour. The
specificity of gene therapy in identifying and destroying cancer cells may make
it a more attractive option than conventional chemotherapy which can
indiscriminately kill healthy cells along with cancerous ones.
Cytokines, Interferons
and Interleukins
Cytokines are small proteins
that are similar to hormones. They have specific effects on the behaviour of
other cells. Interleuken-2 (IL2), which was initially identified in 1976 and has
been used in treatment of AIDS, is one such protein. IL2 stimulates the growth
of T-cells. T-cells are a type of immune system cell, sometimes referred to as
"killer cells" because they search out and destroy malignant or virally infected
cells. Using IL2 as a treatment for pleural mesothelioma is still in the
experimental stages, but researchers hope that injecting IL2 intra-pleurally
will prove to promote a significant anti-tumour response.
To date, however, IL2 and
interferon-gamma (IFN-gamma), a similar substance, have produced limited results
and substantial adverse effects. IFN-gamma did produce good results when used in
a study of 89 patients with early stage mesothelioma. Over 46 months of
treatment, there was an overall response rate of 20%. Nine percent of those had
complete responses, and an additional ten percent experienced at least a 50%
reduction in the size of their tumours. In this study, patients who entered
during Stage I of their disease fared the best, reporting a response rate of
45%.
Another immunotherapy agent,
IFN-alpha-2a, was found have some limited efficacy, one complete response and
three partial responses in a group of 25 patients who received the agent
subcutaneously. IFN-alpha-2a did not produce significant side effects in that
study.
Finally, significant
regression of mesothelioma has been reported from direct injection of the
immunotherapy agent GM-CSF into the tumour on a regular basis.
Photodynamic therapy
Photodynamic therapy uses
light to kill cancerous cells. The patient receives a photosensitizing drug--
which targets cancer cells and renders them vulnerable to light of specific
wavelengths. After the drug has sensitized the cancerous cells, fibreoptic
cables are placed in the body (usually through open-chest surgery). The
fibreoptic cables direct light of a precisely adjusted frequency onto the
tumour. This causes the photosensitizing drug to produce a toxic oxygen
molecule, which kills the cancer cell.
Patients who undergo this type
of therapy often do so following surgery and chemotherapy.
Although this treatment is
still in a very experimental stage for the treatment of mesothelioma, it has
shown promising results in the treatment of other cancers.
BACK



