|
Soft Tissue Sarcoma
Adult soft tissue sarcoma is a disease in
which cancer (malignant) cells are found in the soft tissue of part of the body.
The soft tissues of the body include the muscles, connective tissues (tendons),
vessels that carry blood or lymph, joints, and fat.
A lump or swelling in part of the body may appear if a person has a soft tissue sarcoma. The lump may not be painful. If there are symptoms, a doctor may cut out a piece of tissue from the swollen area. This is called a biopsy. The tissue will be looked at under a microscope to see if there are any cancer cells. A patient may need to go to the hospital for this test. The chance of recovery (prognosis) and choice of treatment depend on the size and stage of the cancer (how far the cancer has spread), and the patientís age and general health. Stages of adult soft tissue sarcoma
|
|
|
Ewingís family of tumours
The Ewingís family of tumours include: Ewingís
tumour of bone; extraosseus Ewingís (tumour growing outside of the bone);
primitive neuroectodermal tumour (PNET), also known as peripheral
neuroepithelioma; and Askinís tumor (PNET of the chest wall). These tumours are
rare diseases in which cancer (malignant) cells are found in the bone and soft
tissues. Ewingís family of tumours most frequently occurs in teenagers.
If a patient has symptoms (such as pain, stiffness, or tenderness in the bone) the doctor may order x-rays and other tests. The doctor may also cut out a piece of tissue from the affected area. This is called a biopsy. The tissue will be looked at under a microscope to see if there are any cancer cells. This test may be done in the hospital. The chance of recovery (prognosis) and choice of treatment depend on the location, size, and stage of the cancer (how far the cancer has spread), how the cancer cells react to the treatment, and the patientís age and general health. Stages of the Ewingís family of tumours
|
How the Ewingís family of tumours are
treated
|
Kaposiís sarcoma (KS) is a disease in which
malignant cells are found in the tissues under the skin or mucous membranes that
line the mouth, nose, and anus. KS causes red or purple patches (lesions) on the
skin and/or mucous membranes and spreads to other organs in the body, such as
the lungs, liver, or intestinal tract.

Until the early 1980ís, Kaposiís sarcoma was a very rare disease that was found mainly in older men, patients who had organ transplants, or African men. With the Acquired Immunodeficiency Syndrome (AIDS) epidemic in the early 1980ís, doctors began to notice more cases of Kaposiís sarcoma in Africa and in gay men with AIDS. Kaposiís sarcoma usually spreads more quickly in these patients.
If there are signs of KS, a doctor will examine the skin and lymph nodes carefully (lymph nodes are small bean-shaped structures that are found throughout the body; they produce and store infection-fighting cells). The doctor also may order other tests to see if the patient has other diseases.
The chance of recovery (prognosis) depends on what type of Kaposiís sarcoma the patient has, the patientís age and general health, and whether or not the patient has AIDS.
Radiation therapy is a common treatment of Kaposiís sarcoma. Radiation therapy uses high-dose x-rays or other high-energy rays to kill cancer cells and shrink tumours. Radiation for Kaposiís sarcoma comes from a machine outside the body (external beam radiation therapy).
Surgery means taking out the cancer. A doctor may remove the cancer using one of the following:
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken by pill, or it may be put into the body by a needle in a vein or muscle. Chemotherapy is called a systemic treatment because the drug enters the bloodstream, travels through the body, and can kill cancer cells outside the original site. Chemotherapy for Kaposiís sarcoma also may be injected into the lesion (intra-lesional chemotherapy).
Biological therapy tries to get the body to fight the cancer. It uses materials made by the body or made in a laboratory to boost, direct, or restore the bodyís natural defences against disease. Biological therapy is sometimes called biological response modifier (BRM) therapy or immunotherapy.
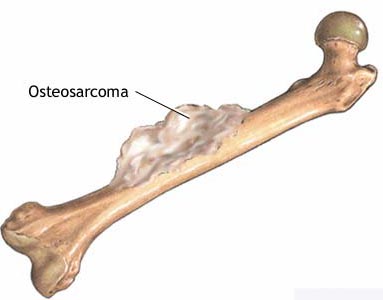
Osteosarcoma is a disease in which malignant
cells are found in the bone. It is the most common type of bone cancer. In
children, it occurs most commonly in the bones around the knee. Osteosarcoma
most often occurs in adolescents and young adults.
Malignant fibrous histiocytoma of bone (MFH) is a rare tumour of the bone. It may occur following radiation treatments. MFH is generally treated the same as osteosarcoma and appears to have a similar response to treatment.
If a patient has symptoms (such as pain and swelling of a bone or a bone region), a doctor may order x-rays and blood tests. If it is suspected that the problem is osteosarcoma, your doctor may recommend seeing a specialist called an orthopaedic oncologist. The orthopaedic oncologist may cut out a piece of tissue from the affected area. This is called a biopsy. The tissue will be looked at under a microscope to see if there are any cancer cells. This test may be done in the hospital.
The chance of recovery (prognosis) and choice of treatment depend on the size, location, type, and stage of the cancer (how far the cancer has spread), how long the patient had symptoms, how much of the cancer is taken out by surgery and/or killed by chemotherapy, and the patientís age, blood and other test results, and general health.
There are treatments for all patients with osteosarcoma. Three kinds of treatment are used:
Surgery is a common treatment for osteosarcoma. The doctor may remove the cancer and some of the healthy tissue around the cancer. Sometimes all or part of an arm or leg may have to be removed (amputated) to make sure that all of the cancer is taken out. If cancer has spread to lymph nodes, the lymph nodes will be removed (lymph node dissection).
In patients with osteosarcoma that has not spread beyond the bone, researchers are studying whether surgery without amputation of the arm or leg (limb-sparing procedures) can be done without the cancer coming back. Sometimes the cancer can be taken out without amputation, and artificial devices or bones from other places in the body can be used to replace the bone that was removed.
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken by pill or put into the body by a needle in a vein or muscle. Chemotherapy is called systemic treatment because the drug enters the blood stream, travels through the body, and can kill cancer cells throughout the body. Chemotherapy with more than one drug is called combination chemotherapy.
Sometimes chemotherapy is injected directly into the area where the cancer is found (regional chemotherapy). In osteosarcoma, surgery is often used to remove the local tumour and chemotherapy is then given to kill any cancer cells that remain in the body. Chemotherapy given after surgery has removed the cancer is called adjuvant chemotherapy. Chemotherapy can also be given before surgery to shrink the cancer so that it can be removed during surgery; this is called neo-adjuvant chemotherapy.
Radiation therapy uses x-rays or other high-energy rays to kill cancer cells and shrink tumours. Radiation for osteosarcoma usually comes from a machine outside the body (external radiation therapy).
Treatment for osteosarcoma depends on the stage of the disease, where the cancer is found, and the patientís age and general health
Treatment of malignant fibrous histiocytoma of bone may be the following:
Osteosarcoma
Treatment may be one of the following:
Surgery often includes removal of cancer that has spread to the lungs.
Malignant fibrous histiocytoma of bone
The standard treatments for patients with
unresectable or metastatic malignant fibrous histiocytoma of bone have not yet
been determined.
If the cancer has come back only in the lungs, treatment may be surgery to remove the cancer in the lungs with or without chemotherapy. If the cancer has come back in other places besides the lungs, treatment may be combination chemotherapy. Clinical trials are evaluating new chemotherapy drugs.