|
Malignant Melanoma
Melanoma is a disease in which malignant
(cancer) cells form in the skin cells called melanocytes (cells that colour the
skin). Melanocytes are found throughout the lower part of the epidermis. They
produce melanin, the pigment that gives skin its natural colour. When skin is
exposed to the sun, melanocytes produce more pigment, causing the skin to tan,
or darken. 
The skin is the bodyís largest organ. It protects against heat, sunlight,
injury, and infection. The skin has 2 main layers: the epidermis (upper or outer
layer) and the dermis (lower or inner layer).
When melanoma starts in the skin, the disease is called cutaneous melanoma.
Melanoma may also occur in the eye and is called ocular melanoma or intraocular
melanoma.
Melanoma can occur anywhere on the body. In men, melanoma is often found on the
trunk (the area from the shoulders to the hips) or the head and neck. In women,
melanoma often develops on the arms and legs. Melanoma usually occurs in adults,
but it is sometimes found in children and adolescents. Unusual moles, exposure
to sunlight, and health history can affect the risk of developing melanoma. Risk factors include the following: affect the risk of developing melanoma. Risk factors include the following:
-
Unusual moles
-
Exposure to natural sunlight,
including sunburns during childhood
-
Exposure to artificial
ultraviolet light (tanning machines)
-
Family or personal history of
melanoma
-
Red or blond hair
-
White or light-coloured skin and
freckles
-
Blue eyes
Possible signs of melanoma include a change in
the appearance of a mole or pigmented area. These and other symptoms may be
caused by melanoma or by other conditions. A doctor should be consulted if any
of the following problems occur:
- A mole that: changes in size, shape, or
colour; has irregular edges or borders; is more than 1 colour; is asymmetrical
ie if the mole is divided in half, the 2 halves are different in size or
shape; itches; oozes, bleeds, or is ulcerated - a hole forms in the skin when
the top layer of cells breaks down and the underlying tissue shows through.
- Change in pigmented (coloured) skin.
- Satellite moles (new moles that grow
near an existing mole)
Tests that examine the skin are used to detect
and diagnose melanoma. If a mole or pigmented area of the skin changes or
looks abnormal, the following tests and procedures can help detect and diagnose
melanoma:
Skin examination: A doctor or nurse examines
the skin to look for moles, birthmarks, or other pigmented areas that look
abnormal in colour, size, shape, or texture.

Biopsy: A local excision is done to remove as
much of the suspicious mole or lesion as possible. A pathologist then looks at
the tissue under a microscope to check for cancer cells. Because melanoma can be
hard to diagnose, patients should consider having their biopsy sample checked by
a second pathologist.
Suspicious areas should not be shaved off or cauterized (destroyed with a hot
instrument, an electrical current, or a caustic substance).
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on the
following:
- The stage of melanoma (whether cancer is
found in the outer layer of skin only, or has spread to the lymph nodes or to
other places in the body).
- Whether there was bleeding or ulceration at
the primary site.
- The location and size of the tumour.
- The patientís general health.
Although many people are successfully
treated, melanoma can recur
Stages of Melanoma
After melanoma has been diagnosed, tests are done to find out if cancer cells
have spread within the skin or to other parts of the body. The process used to
find out whether cancer has spread within the skin or to other parts of the body
is called staging. The information gathered from the staging process determines
the stage of the disease. It is important to know the stage in order to plan
treatment.
The following tests and procedures may be used in the staging process:
- Wide local excision: A surgical procedure
to remove some of the normal tissue surrounding the area where melanoma was
found, to check for cancer cells.
- Lymph node mapping and sentinel lymph node
biopsy: Procedures in which a radioactive substance and/or blue dye is
injected near the tumour. The substance or dye flows through lymph ducts to
the sentinel node or nodes (the first lymph node or nodes where cancer cells
are likely to have spread). The surgeon removes only the nodes with the
 radioactive substance or dye. A pathologist then checks the sentinel lymph
nodes for cancer cells. If no cancer cells are detected, it may not be
necessary to remove additional nodes.
radioactive substance or dye. A pathologist then checks the sentinel lymph
nodes for cancer cells. If no cancer cells are detected, it may not be
necessary to remove additional nodes.
- Chest x-ray: An x-ray of the organs and
bones inside the chest. An x-ray is a type of energy beam that can go through
the body and onto film, making a picture of areas inside the body.
- CT scan (CAT scan): A procedure that makes
a series of detailed pictures of areas inside the body, taken from different
angles. The pictures are made by a computer linked to an x-ray machine. A dye
may be injected into a vein or swallowed to help the organs or tissues show up
more clearly. This procedure is also called computed tomography, computerized
tomography, or computerized axial tomography. For melanoma, pictures may be
taken of the chest, abdomen, and pelvis.
- MRI (magnetic resonance imaging): A
procedure that uses a magnet, radio waves, and a computer to make a series of
detailed pictures of areas inside the body. This procedure is also called
nuclear magnetic resonance imaging (NMRI).
- PET scan (positron emission tomography
scan): A procedure to find malignant tumour cells in the body. A small amount
of radionuclide glucose (sugar) is injected into a vein. The PET scanner
rotates around the body and makes a picture of where glucose is being used in
the body. Malignant tumour cells show up brighter in the picture because they
are more active and take up more glucose than normal cells.
- Laboratory tests: Medical procedures that
test samples of tissue, blood, urine, or other substances in the body. These
tests help to diagnose disease, plan and check treatment, or monitor the
disease over time.
The results of these tests are viewed together
with the results of the original tumour biopsy to determine the melanoma stage.
The following stages are used for melanoma:
Stage 0
In stage 0, melanoma is found only in the epidermis (outer layer of the skin).
Stage 0 is also called melanoma in situ.
Stage I
Stage I is divided into stages IA and IB.
Stage IA
In stage IA, the tumour is not more than
1 millimetre (less than 1/16 of an inch) thick, with no ulceration (a hole that
forms in the skin when the top layer of cells breaks down and the underlying
tissue shows through). The tumour is in the epidermis and upper layer of the
dermis.
Stage IB
In stage IB, the tumour is either: not more
than 1 millimetre thick, with ulceration, and may have spread into the dermis or
the tissues below the skin; or
1 to 2 millimetres (more than 1/16 inch) thick, with no ulceration.
Stage II
Stage II is divided into stages IIA, IIB, and IIC.
Stage IIA
In stage IIA, the tumour is either: 1 to 2
millimetres thick, with ulceration; or
2 to 4 millimetres (a little more than 1/8 of an inch) thick, with no
ulceration.
Stage IIB
In stage IIB, the tumour is either: 2 to 4
millimetres thick, with ulceration; or
more than 4 millimetres thick, with no ulceration.
Stage IIC
In stage IIC, the tumour is more than 4
millimetres thick, with ulceration.
Stage III
In stage III, the tumour may be of any thickness, with or without ulceration,
and may have spread to 1 or more nearby lymph nodes. Stage III is divided into
stages IIIA, IIIB, and IIIC.
Stage IIIA
In stage IIIA, the cancer may have spread to
as many as 3 nearby lymph nodes, but can only be seen with a microscope.
Stage IIIB
In stage IIIB, the cancer either: has spread
to as many as 3 lymph nodes and may not be visible without a microscope; or has
satellite tumours (additional tumour growths within 1 inch of the original
tumour) and has not spread to lymph nodes.
Stage IIIC
In stage IIIC, the cancer either: has spread
to as many as 4 or more lymph nodes and can be seen without a microscope; or has
lymph nodes that may not be moveable; or
has satellite tumours and may have spread to lymph nodes.
Stage IV
In stage IV, the tumour has spread to other organs or to lymph nodes far away
from the original tumour.
Recurrent Melanoma
Recurrent melanoma is cancer that has recurred (come back) after it has been
treated. The cancer may come back in the original site or in other parts of the
body, such as the lungs or liver.
Treatment for patients with melanoma
Different types of treatment are available for patients with melanoma. Some
treatments are standard (the currently used treatment), and some are being
tested in clinical trials. Before starting treatment, patients may want to think
about taking part in a clinical trial. A treatment clinical trial is a research
study meant to help improve current treatments or obtain information on new
treatments for patients with cancer. When clinical trials show that a new
treatment is better than the "standard" treatment, the new treatment may become
the standard treatment.
Four types of standard treatment are used:
- Surgery
- Surgery to remove the tumour is the primary
treatment of all stages of melanoma. The doctor may remove the tumour using
the following operations:
- Local excision: Taking out the melanoma and
some of the normal tissue around it.
Wide local excision with or without removal of lymph nodes.
- Lymphadenectomy: A surgical procedure in
which the lymph nodes are removed and examined to see whether they contain
cancer.
- Sentinel lymph node biopsy: The removal of
the sentinel lymph node (the first lymph node the cancer is likely to spread
to from the tumour) during surgery. A radioactive substance and/or blue dye is
injected near the tumour. The substance or dye flows through the lymph ducts
to the lymph nodes. The first lymph node to receive the substance or dye is
removed for biopsy. A pathologist views the tissue under a microscope to look
for cancer cells. If cancer cells are not found, it may not be necessary to
remove more lymph nodes.
- Skin grafting (taking skin from another
part of the body to replace the skin that is removed) may be done to cover the
wound caused by surgery.
Even if the doctor removes all the melanoma that can be seen at the time of the
operation, some patients may be offered chemotherapy after surgery to kill any
cancer cells that are left. Chemotherapy given after surgery, to increase the
chances of a cure, is called adjuvant therapy.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer
cells, either by killing the cells or by stopping the cells from dividing. When
chemotherapy is taken by mouth or injected into a vein or muscle, the drugs
enter the bloodstream and can reach cancer cells throughout the body (systemic
chemotherapy). When chemotherapy is placed directly in the spinal column, a body
cavity such as the abdomen, or an organ, the drugs mainly affect cancer cells in
those areas.
In treating melanoma, chemotherapy drugs may be given as a hyperthermic isolated
limb perfusion. This technique sends anticancer drugs directly to the arm or leg
in which the cancer is located. The flow of blood to and from the limb is
temporarily stopped with a tourniquet, and a warm solution containing anticancer
drugs is put directly into the blood of the limb. This allows the patient to
receive a high dose of drugs in the area where the cancer occurred. The way the
chemotherapy is given depends on the type and stage of the cancer being treated.
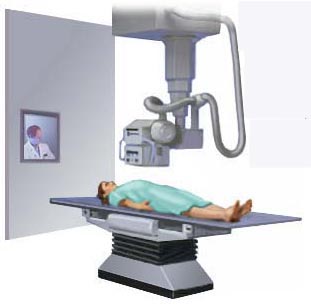
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other
types of radiation to kill cancer cells. There are two types of radiation
therapy. External radiation therapy uses a machine outside the body to send
radiation toward the cancer. Internal radiation therapy uses a radioactive
substance sealed in needles, seeds, wires, or catheters that are placed directly
into or near the cancer. The way the radiation therapy is given depends on the
type and stage of the cancer being treated.
Biologic therapy
Biologic therapy is a treatment that uses the patientís immune system to fight
cancer. Substances made by the body or made in a laboratory are used to boost,
direct, or restore the bodyís natural defences against cancer. This type of
cancer treatment is also called biotherapy or immunotherapy.
Other types of treatment are being tested in clinical trials.
Chemoimmunotherapy is the use of anticancer drugs combined with biologic therapy
to boost the immune system to kill cancer cells.
Treatment Options By Stage
Stage 0 Melanoma
Treatment of stage 0 melanoma is usually surgery to remove the tumour and a
small amount of normal tissue around it.
Stage I Melanoma
Treatment of stage I melanoma may include the following:
- Surgery to remove the tumour and some of
the normal tissue around it.
- A clinical trial of surgery to remove the
tumour and some of the normal tissue around it, with or without lymph node
mapping and selective lymphadenectomy.
- A clinical trial of new techniques to
detect cancer cells in the lymph nodes.
- A clinical trial of lymphadenectomy with or
without adjuvant therapy.
Stage II Melanoma
Treatment of stage II melanoma may include the following:
- Surgery to remove the tumour and some of
the normal tissue around it, followed by removal of nearby lymph nodes.
- Lymph node mapping and sentinel lymph node
biopsy, followed by surgery to remove the tumour and some of the normal tissue
around it. If cancer is found in the sentinel lymph node, a second surgical
procedure can be performed to remove additional nearby lymph nodes.
- Surgery followed by high-dose biologic
therapy.
- A clinical trial of adjuvant chemotherapy
and/or biologic therapy, or immunotherapy.
- A clinical trial of new techniques to
detect cancer cells in the lymph nodes.
Stage III Melanoma
Treatment of stage III melanoma may include the following:
- Surgery to remove the tumour and some of
the normal tissue around it.
- Surgery to remove the tumour with skin
grafting to cover the wound caused by surgery.
- Surgery followed by biologic therapy.
- A clinical trial of surgery followed by
chemotherapy and/or biologic therapy.
- A clinical trial of biologic therapy.
- A clinical trial comparing surgery alone to
surgery with biologic therapy.
- A clinical trial of chemoimmunotherapy or
biologic therapy.
- A clinical trial of hyperthermic isolated
limb perfusion using chemotherapy and biologic therapy.
- A clinical trial of biologic therapy and
radiation therapy.
Stage IV Melanoma
Treatment of stage IV melanoma may include the following:
- Surgery as palliative therapy to relieve
symptoms and improve quality of life.
- Radiation therapy as palliative therapy to
relieve symptoms and improve quality of life.
- Chemotherapy and/or biologic therapy.
- A clinical trial of new chemotherapy and/or
biologic therapy, or vaccine therapy.
- A clinical trial of radiation therapy as
palliative therapy to relieve symptoms and improve quality of life.
- A clinical trial of surgery to remove all
known cancer.
Treatment Options for Recurrent Melanoma
Treatment of recurrent melanoma may include the following:
- Surgery to remove the tumour.
- Radiation therapy as palliative therapy to
relieve symptoms and improve quality of life.
- Palliative treatment with biologic therapy.
- Hyperthermic isolated limb perfusion.
- A clinical trial of biologic therapy and/or
chemotherapy as palliative therapy to relieve symptoms and improve quality of
life.
BACK
|





