|
What is radiotherapy?
Since the discovery of x-rays over one hundred
years ago, radiation has been used increasingly in medicine, both to help with
diagnosis (by taking pictures with x-rays), and as a treatment (radiotherapy).
While radiation obviously has to be used with care, doctors and radiographers
have great experience in its use in medicine.
 Radiotherapy treatment can cure some cancers
and can reduce the chance of a cancer coming back after surgery, but can cause
side effects. It can be used to reduce cancer symptoms. The benefits and
possible side effects are discussed in detail below. Radiotherapy treatment can cure some cancers
and can reduce the chance of a cancer coming back after surgery, but can cause
side effects. It can be used to reduce cancer symptoms. The benefits and
possible side effects are discussed in detail below.
Radiotherapy is the use of x-rays and similar
rays (such as photons) to treat disease. Many people with cancer will have
radiotherapy as part of their treatment. This can be given either as external
radiotherapy from outside the body, using x-rays or
cobalt irradiation, or from within the body as
internal radiotherapy.
Radiotherapy works by destroying the cancer
cells in the treated area. Although normal cells are also sometimes damaged by
the radiotherapy, they can repair themselves more effectively.
External radiotherapy
External radiotherapy is normally given as a
series of short daily treatments in the radiotherapy department, using equipment
similar to a large x-ray machine. department, using equipment
similar to a large x-ray machine.
The treatments are usually given from Monday
to Friday, leaving patients to rest at the weekend. Each treatment is called a
fraction. Giving the treatment in fractions ensures that less damage is
done to normal cells than to cancer cells. The damage to normal cells is mainly
temporary, but is the reason why radiotherapy has some side effects.

The number of treatments you have depends on
several factors, including:
- your general health
- the site and type of cancer being treated
- whether or not you have had, or are going
to have, surgery, chemotherapy or hormonal therapy as part of your treatment.
For these reasons, treatment is planned for
each patient individually, and even people with the same type of cancer may have
different treatments.
External radiotherapy does not make you
radioactive, and it is perfectly safe for you to be with other people, including
children, throughout your treatment.
A course of curative (radical) treatment may
be given every weekday from two to six weeks. Instead of having one treatment a
day or having a rest at the weekend, some people will have different treatment
plans. They may have more than one treatment a day or treatment every day for
two weeks. Giving radiotherapy in this way is known as continuous
hyperfractionated radiotherapy (often called CHART).
Sometimes treatment may be given on only three
days each week (for example, on Mondays, Wednesdays and Fridays). Palliative treatment (for symptom control) may
involve only one or two sessions of treatment, or up to five sessions.
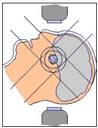
The different types of radiotherapy machine
work in slightly different ways. Some are better for treating cancers near the
surface of the skin, while others work best on cancers deeper in the body.
 The
type of radiotherapy machine used will be carefully chosen by your specialist
and physicist to give you the most appropriate treatment. Some machines are
quicker than others and may give treatment in a very short time, such as a few
seconds. Usually, radiotherapy treatment (including the time taken to position
you) takes 10-15 minutes or less, on any machine. The
type of radiotherapy machine used will be carefully chosen by your specialist
and physicist to give you the most appropriate treatment. Some machines are
quicker than others and may give treatment in a very short time, such as a few
seconds. Usually, radiotherapy treatment (including the time taken to position
you) takes 10-15 minutes or less, on any machine.
The radiotherapy machine does not normally
touch you and the treatment itself is painless, although it may gradually cause
some uncomfortable side effects. If you have a specific type of radiotherapy
known as electron treatment, a small applicator may be used, which touches a
small area of skin.
People react to radiotherapy in different
ways: some find that they can carry on working, taking time off for their
treatment, while others find it too tiring and prefer to stay at home. If you
have a family to look after, you may find that you need extra help. Don't be
afraid to ask for help, whether it's from your employer, family or friends,
social services, or the staff in the radiotherapy department. As your treatment
progresses, you will have a better idea of how it makes you feel so you can make
any necessary changes to your daily life.
The radiotherapy staff will try to give you an
appointment for the same time each day. This gives your body a chance to recover
from any side effects between treatments and also allows you to get into a daily
routine.
Internal radiotherapy
Internal radiotherapy is used mainly to treat cancers in the head and neck area,
the cervix, the womb, the prostate gland or the skin.
Treatment is given in one of two ways: either by putting solid radioactive
material (the source) close to or inside the tumour for a limited period of
time, or by using a radioactive liquid, which the patient takes either as a
drink or as an injection into a vein.
If you have internal radiotherapy, you may have to stay in hospital for a few
days and some special precautions will have to be taken while the radioactive
material is in place in your body. Once the treatment is over there is no risk
of exposing your family or friends to radiation.
The process of putting solid radioactive material close to or inside the tumour
is called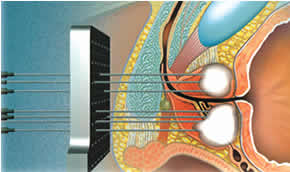 brachytherapy.
Giving a radioactive liquid, either as a drink, in a capsule or given as an
injection into a vein is called radioisotope treatment. Your specialist will
discuss your particular treatment with you. Before having your treatment you
will be asked to sign a form to say that you give your permission. brachytherapy.
Giving a radioactive liquid, either as a drink, in a capsule or given as an
injection into a vein is called radioisotope treatment. Your specialist will
discuss your particular treatment with you. Before having your treatment you
will be asked to sign a form to say that you give your permission.
Radioactive isotopes
Because of the possibility of unnecessary radiation exposure to the hospital
staff and your friends and relatives, certain safety measures are taken while
you are being treated with the radioactive source, or after you have been given
a liquid radioisotope. Depending on the type of treatment you are receiving,
this means the restrictions may be needed for a few days. But sometimes they are
only needed for a few minutes.
The staff looking after you will explain these restrictions to you in more
detail before you start your treatment. Each hospital has different routines,
and it is worth visiting beforehand to discuss what will happen with the nursing
and medical staff.
You may be admitted to the ward the day before your treatment so the staff can
go over the procedure with you. This is a good time to ask questions and it may
help to make a list beforehand so you don't forget something important.
While the radioactive source is in place, or after treatment with a liquid
radioisotope:
You will probably be nursed in a side room, away from the main ward. You may be
nursed alone or with someone else having similar treatment. Lead screens may be
placed on either side of your bed to absorb any radiation that is given out. The
doctors and staff on the ward will only stay in your room for short periods at a
time. Staff and visitors will be asked to stand away from your bed to reduce
their exposure to the rays.
If you are being treated with a radioactive source, the safety measures are only
necessary while it is in place. Before and after your treatment, your visitors
can come at normal visiting times.
 Some people worry that they will remain radioactive once the treatment is over,
and be dangerous to their family and friends. If you have been treated with a
radioactive source, this is not so. As soon as the radioactive source has been
removed, all traces of radiation disappear. Some people worry that they will remain radioactive once the treatment is over,
and be dangerous to their family and friends. If you have been treated with a
radioactive source, this is not so. As soon as the radioactive source has been
removed, all traces of radiation disappear.
If you have been given a liquid treatment, however, the radioactivity will
disappear gradually. Before you leave hospital the staff will check that most of
the radioactivity in your body has gone, and that your belongings are free of
any signs of radioactivity. After you leave hospital you should be able to carry
on your life almost as normal, but there may be a few restrictions about meeting
people - especially children and pregnant women - for a few more days.
Caesium insertion
This type of internal radiotherapy treatment is used for treating cancer of the
cervix, uterus or vagina. The radioactive source most commonly used is called
caesium-137. The advantage of caesium insertion treatment is that it gives a
high dose of radiotherapy directly to the tumour, but gives a low dose to normal
tissues.
The caesium source has to be put inside an applicator (there may be more than
one) to keep it in place. The applicator, is inserted into the vagina, while you
are under a general anaesthetic or sedation in the operating room. At the same
time, a flexible tube called a urinary catheter may be put into your bladder to
drain off urine. This means you don't have to get on and off bedpans and risk
moving the applicators. Once the applicators are in place an X-ray will be taken
to check they are in the correct position. Sometimes the radioactive source is
put into the applicator while you are in the operating room, but more commonly
it will be put in place once you are back on the ward. You may hear this
referred to as 'afterloading'.
The applicators are kept in place by a pack (cotton/gauze padding) inside your
vagina. This can be uncomfortable and you may need to ask your nurse for regular
painkillers.
Once the source is put into the applicators you have to stay in bed. This helps
to keep them in the correct position. If you need anything, you can call a
member of staff by using the call bell by your bed. If the source does get
dislodged, you should call the staff on the ward immediately.
 Curitron/Selectron machine Curitron/Selectron machine
In some hospitals a machine, which may be called a Curitron or Selectron or
similar name, is used to put the radioactive material into the applicators. The
machine is attached by tubes to the applicators. When the machine is switched on
it passes small radioactive sources into the applicators. If the machine is
switched off, the source is pulled back inside the machine. The machine is kept
switched on throughout your treatment, except when someone needs to go into your
room. It can then be turned off, so reducing their exposure to the rays.
However, safety measures and visiting restrictions are still necessary. The time
you spend on the machine varies but it is usually between 12 and 48 hours.
Microselectron
Sometimes a machine called a Microselectron can be used to give internal
radiotherapy. This gives the radiotherapy more quickly, so the treatments last
for only a few minutes and you can go home the same day.
After the treatment
Once you have received your dose of radiation the sources and the applicators
will be removed. This is usually done on the ward. As it can be a little
uncomfortable, you will be offered some painkillers beforehand. Sometimes a few
breaths of the gas Entonox will help you to relax. The staff on the ward check
that all the applicators and sources have been removed. Your catheter may be
removed at the same time.
Your doctor may suggest you use vaginal douches for a few days after the
insertion has been removed to keep the vagina clean. Your nurse will show you
how to use these. You will probably be able to go home the same, or the
following, day. Once the radioactive sources are removed, all traces of
radioactivity will immediately disappear.
Side effects
Many women will be treated with both internal and external radiotherapy to
ensure the area is treated in the most effective way.
There is a slight risk of infection following caesium insertion but this is very
rare. If you do develop a high temperature or heavy bleeding after your
treatment you should contact your doctor as soon as possible. You will be
prescribed antibiotics to deal with the infection.
Caesium or iridium implants
These can be used to treat a number of tumours including those in the mouth, lip
and breast. Very fine needles, wires or tubes carry the radioactive source, and
are inserted while you are in the operating room under a general anaesthetic.
An X-ray may be taken to ensure that they are in the correct position. You will
be nursed in a separate room, and safety measures will be applied until the
wires are removed, usually between three and eight days. Sometime this is done
under general anaesthetic.
Implants in the mouth can be uncomfortable, and can make eating and talking
difficult. A soft or liquid diet may be necessary while the needles are in
place. Your nurse will show you how to keep your mouth clean, using regular
mouthwashes. If eating is a problem you may be fed through a thin tube (nasogastric
tube) which is passed via your nose and into your stomach.
The implant is removed once the correct dose of radiation has been received.
This may be after two days, if the treatment is given as a booster after
external treatment, or up to one week if given as the only form of treatment.
Once the implant has been removed the area will feel sore for up to two or three
weeks afterwards. Your specialist will prescribe pain killers that you can take
regularly until this improves.
 Radioactive seed implants are occasionally used to treat small tumours of the
prostate gland. See the section on cancer of the prostate that explains this
treatment in more detail. Radioactive seed implants are occasionally used to treat small tumours of the
prostate gland. See the section on cancer of the prostate that explains this
treatment in more detail.
Radioactive isotopes
These are given as liquids, either through the mouth (in capsules or as a drink)
or by injection into a vein (called an intravenous injection). The commonest
form of radioisotope treatment is radio-iodine. It is used to treat tumours of
the thyroid gland, and is given in the form of an odourless and colourless
drink.
The same safety precautions will be taken with this type of treatment as with
implants.
Any radio-iodine which is not absorbed by your thyroid will be passed from the
body in sweat and urine. You should drink plenty of fluids during your treatment
as this helps to flush the iodine out of the body. The amount of radiation in
your body will be checked regularly and as soon as it falls to a safe level,
after about four to seven days, you will be able to go home. You may need to
take some special precautions for a short time after going home - particularly
with young children and pregnant women. The hospital staff will explain these to
you.
Radioisotope treatment can also be given when certain types of cancer have
spread to the bones (secondary cancer in the bone). A radioisotope is injected
into a vein and this is normally given as an out-patient. Before you go home you
will be given some simple advice to follow as your urine and blood are slightly
radioactive for a few days. The section
on secondary bone cancer has more information on this treatment.
More on Side Effects
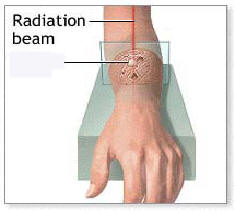
Cancer cells usually multiply
faster than other cells in the body. Since radiation is most harmful to rapidly
reproducing cells, radiation damages cancer cells more than the normal cells of
the body. It prevents these cells from continuing to reproduce and thus prevents
the tumour from growing further.
 Unfortunately, rapidly dividing healthy cells can also be killed by this
process. Skin and hair are some of the tissues most noticeably affected by
radiation treatment, resulting in skin lesions, burning, redness, and possibly
hair loss. Unfortunately, rapidly dividing healthy cells can also be killed by this
process. Skin and hair are some of the tissues most noticeably affected by
radiation treatment, resulting in skin lesions, burning, redness, and possibly
hair loss.
Radiation therapy is used to fight many types of cancer. Often it is used to
shrink the tumour as much as possible before surgery to remove the cancer.
Radiation can also be given after surgery to prevent the cancer from coming
back.
For certain types of cancer, radiation is the only treatment needed. Radiation
treatment may also be used to provide temporary relief of symptoms, or to treat
malignancies (cancers) that cannot be removed with surgery.
The following are some commonly used radioactive substances:
Caesium (137Cs) -
Cobalt (60Co) -
Iodine (131I) -
Phosphorus (32P)
Gold (198Au) -
Iridium (192Ir) -
Yttrium (90Y) -
Palladium (109)
Radiation therapy can have many
side effects. These side effects depend on the part of the body being irradiated
and the dose and schedule of the radiation:
Fatigue and malaise
Low blood counts
Difficulty or pain swallowing
Erythema
Oedema
The shedding or sloughing-off of the outer layer of skin (desquamation)
Increased skin pigment (hyper-pigmentation)
Atrophy
Skin itching (pruritus)
Skin pain
Changes in taste
Anorexia
Nausea
Vomiting
Hair loss
Increased susceptibility to infection
Foetal damage (in a pregnant woman) |



